Dr. Sidra Khot
MBBS DGO FRM FMIS
Consultant Obstretician, Laparoscopic Surgeon, and Fertility Specialist
Contact on whatapp +91 9321738667
Email - drsidrakhotclinic@gmail.com
MBBS DGO FRM FMIS
Consultant Obstretician, Laparoscopic Surgeon, and Fertility Specialist
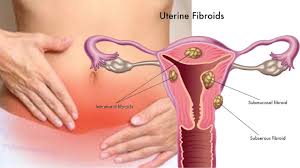
Benign uterine conditions are common in gynecologic patients and often lead to surgeries. Myomas are the most common noncancerous growths in the uterus, affecting 20–25% of women of reproductive age. They can occur in areas with smooth muscle cells, like the uterus, fallopian tubes, or cervix. Myomas result from benign muscle cell growth, influenced by hormones like estrogen and growth hormone. While progesterone may slow their growth, under certain conditions, it can encourage it.
Symptoms
The symptoms of uterine myomas depend on their number, size, and location. Common symptoms include abnormal bleeding, pressure in the abdomen, frequent urination, and constipation. While myomas rarely cause infertility alone, they can contribute to pregnancy loss and preterm birth.
Preoperative Evaluation and Treatment
For patients with heavy bleeding due to myomas, your Doctor will assess anemia using hematocrit levels. Anemic patients may benefit from preoperative hormone therapy like danazol or GnRH agonists to reduce myoma size, restore normal blood levels, and minimize transfusion needs. However, GnRH agonists may have side effects, including a temporary menopausal state, and could increase the chance of myoma recurrence or complicate surgery.
If large myomas in the broad ligament are present, imaging like an intravenous pyelogram may be used to check for ureter obstruction. Pelvic and ultrasound exams can track the growth of myomas. Techniques like hysteroscopy or vaginal ultrasound can detect smaller myomas and guide their removal during surgery.
In some cases, your Doctor may recommend preoperative blood donation to prepare for possible blood loss during surgery. Patients are informed about the risks of bleeding, potential need for blood transfusion, or in rare cases, a hysterectomy.
What are the Risks?
This procedure has a small risk of:
1) Possible removal of the ovary
2) Bleeding that may require a transfusion
3) Infection at the surgical site or bladder
4) Damage to nearby organs like the bladder, bowel, or ureters
5) Potential need for additional surgery
What should I expect during recovery?
After surgery, the abdomen and navel may feel sore or bruised. Shoulder or back pain from the gas used in the procedure is common, as is light vaginal spotting or discharge.
your Doctor will close the incisions with adhesive or dissolvable stitches. Bandages can be removed after 24 hours, and any adhesive strips will fall off on their own or can be removed after seven days. Avoid soaking your incisions in a bath or swimming, but showering is fine as long as you don’t rub the incisions.
You may feel tired in the first week. Rest during this time, and gradually increase your activity with light walks. Resume sexual activity when you feel comfortable.